Blue Light for Rosacea: A Gentler Timeline for Flare Control
Blue light isn’t just for acne, and if you’re someone managing the persistent redness, flushing, or burning sensations of rosacea.
Blue light therapy might offer a calm, non-stripping way to intervene. Especially if your skin reacts poorly to topicals or aggressive treatments, this option speaks softly but effectively.
Blue light therapy can help with rosacea – especially subtype 1 (flushing and redness). Achiving calmness to inflammation and reducing flare-ups when used 2–3 times per week.
Stick to low-irradiance devices, avoid during active flares, and skip if you’re on photosensitizing meds like doxycycline. Always use SPF after treatment to prevent rebound redness.
Here’s what to expect, week by week.
Weeks 1–2 – Soothing Redness By Blue Light Therapy For Rosacea
The first two weeks are all about stabilization – not dramatic overnight shifts, but subtle signals that your skin is less reactive. Clinical studies using 465–470 nm low-irradiance LED arrays observed that skin felt calmer, less tingly, and more tolerant of mild skincare products during early sessions.
“In subjects with facial erythema and neurovascular sensitivity, early blue light exposure decreased visual flushing and improved tactile tolerance.”
Best blue light therapy time:
Start with 2 sessions per week, 10–15 minutes per session.
Panel-style devices or full-face masks are ideal for even coverage, especially across the cheeks and nose – where subtype 1 rosacea tends to flare.
Weeks 3–6 Fewer Flare-Ups and Less Reactivity
Now’s when you start to see the why behind the calm: blue light’s anti-inflammatory effect becomes more visible.
Blue light therapy for rosacea downregulates inflammatory cytokines like IL-1α and TNF-α, which are overexpressed during flare-ups. This not only reduces redness but helps stretch the time between reactive episodes – especially in subtype 1 (erythematotelangiectatic) and some mild subtype 2 cases.
“Controlled blue LED exposure modulated key inflammatory markers without compromising epidermal integrity.”
Consistency tip: Maintain a rhythm of 2–3 sessions per week, and layer on barrier-supporting care (niacinamide, ceramides) after each session to lock in results.
I’ll spotlight two barrier‑friendly heroes – Dr. Dennis Gross DRx and Omnilux Clear Mask – clinically validated to calm redness and reinforce skin resilience.
Long-Term Use – Building Barrier Resilience Safely
The real magic of blue light therapy for rosacea unfolds over months – not days. At around 8–10 weeks, skin often shows improved resilience: redness fades faster, tolerance to new products increases, and those “mystery flares” happen less frequently.
However, it’s not about more, it’s about measured, ongoing care. If you experience rebound dryness or your redness returns quickly post-session, dial back to once weekly or pause for a week.
“Subjects with sensitive-prone skin types maintained flare control with biweekly LED sessions, reporting no epidermal thinning or barrier dysfunction over 12 weeks.”
Bottom line: When used at the right blue light therapy time and dose, blue LED therapy doesn’t just calm rosacea symptoms – it helps reinforce your skin’s natural tolerance over time.
When and How to Use Blue Light Therapy for Rosacea Safely
Blue light therapy for rosacea isn’t a one-size-fits-all treatment – it’s a finesse move. The right protocol can gently calm flare-ups, while the wrong one may push your skin into overdrive. Here’s how to strike the balance.
Ideal Session Frequency and Duration for Sensitive Skin
Start with 2–3 sessions each week, each lasting 5 to 10 minutes. For severely sensitive skin or those in active flare, begin at the lower end of duration.
Clinical observations have shown that low-irradiance protocols (under 20 mW/cm²) applied every other day minimized barrier disruption while still delivering anti-inflammatory effects.
Too much, too fast? Not helpful. Daily treatments, especially in subtype 1 rosacea, can intensify dryness or vascular reactivity. Patience over pressure is key here.
Flip to product cards for insights on Dr. Dennis Gross DRx and Omnilux Clear Mask – no fluff, just rosacea relief.
Preparing the Skin – Cleansing and Topical Compatibility
Let’s keep it minimal:
- Cleanse with a non-foaming, pH-balanced cleanser.
- No actives before your session: omit AHAs, retinoids, salicylic acid, benzoyl peroxide, or anything exfoliating or fragranced.
- Skin should be dry and product-free before light exposure to avoid photoreactive interference or irritation.
Mixing blue light treatment with alcohol-based or exfoliating topicals pre-session resulted in increased skin sensitivity. And decreased barrier recovery time in rosacea-prone users.
If your skin feels tight or warm post-cleansing? Wait a few minutes. Let things settle before switching on your device.
Monitoring Progress and When to Pause Blue Light Therapy For Rosacea
Set real expectations: blue light therapy isn’t instant. Look for:
- Reduced redness and flushing in 2–3 weeks
- Fewer flare-ups and longer “calm periods” by week 4–6
- Better product tolerance over time
But if you notice:
- Increased tightness, itching, or peeling
- Sudden hot spots or post-treatment flushing
- New papules or pustules forming after sessions
Pause immediately. You may be overdoing it or pairing your therapy with incompatible products.
“Users experiencing erythema beyond 30 minutes or persistent stinging should suspend treatment and reassess topical pairings or dosing intervals.” — Phase I Safety Study
Who Should – and Shouldn’t – Try Blue Light for Rosacea
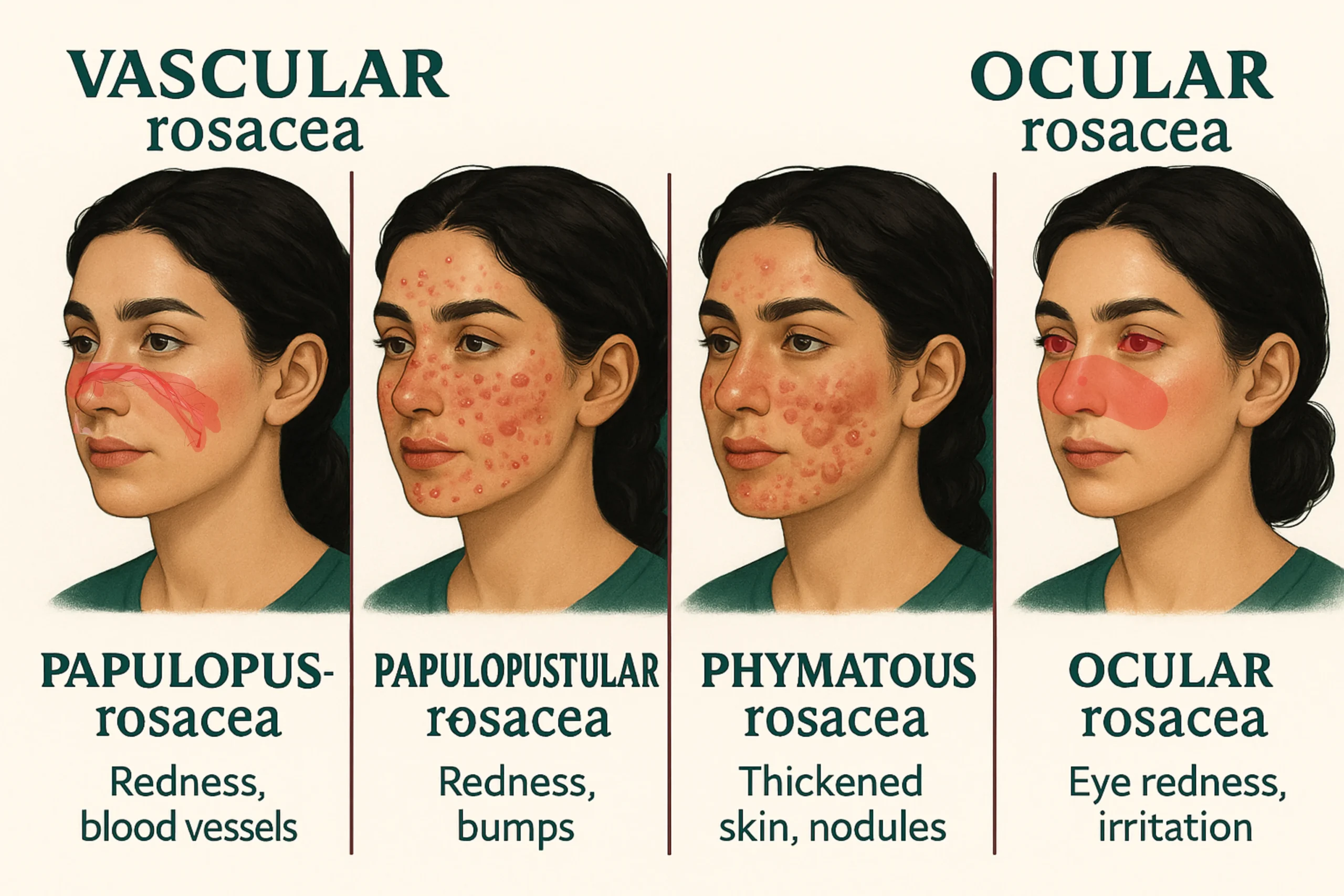
Not all rosacea is created equal—and not every case responds the same way to blue light. Here’s a breakdown of who might benefit most, and who should press pause until they’ve had a proper dermatology consult.
Subtypes That Respond Best to Blue Light
Let’s start with who’s most likely to benefit.
Blue light therapy tends to be most helpful for:
Subtype 1 (erythematotelangiectatic rosacea)
Characterized by flushing, persistent redness, and visible blood vessels. Blue light’s anti-inflammatory qualities and vascular-calming effects may help reduce baseline redness.
Subtype 2 (papulopustular rosacea)
Often confused with adult acne. Here, blue light may help by reducing pro-inflammatory mediators and gently controlling oil – especially when pustules and background redness coexist.
“LED treatment reduced the inflammatory load and frequency of flare cycles in subjects with subtype 1 and 2 rosacea, particularly when paired with barrier-strengthening skincare.” — Photodynamic and Photobiological Effects of LED, 2020
If you experience burning, flushing, or mild pustular activity without the need for prescription medication, you may fall into the sweet spot for light-based support.
Caution in Ocular Rosacea or Severely Dry Skin
Some forms of rosacea require extra caution:
Ocular rosacea
If your symptoms involve eye dryness, redness, or irritation, avoid utilizing blue light near the orbital area—especially without professional assistance. Even with protective goggles, light spillage may increase ocular discomfort.
Severely dry or barrier-compromised skin
If your skin is actively flaking, stinging, or showing signs of atopic dermatitis overlap, blue light may be too stimulating at this point.
Barrier health comes first. Introducing LED treatment too early can prolong inflammation or delay recovery.
“Subjects with impaired barrier function reported increased post-treatment tightness and delayed recovery unless emollient pre-conditioning was implemented.”— A Single-Blind, Dose Escalation, Phase I Study
If in doubt, start with a barrier repair regimen and revisit LED use later.
Don’t miss our product cards see why Dr. Dennis Gross DRx and Omnilux Clear Mask are game‑changers for calming rosacea today.
CONCLUSION
Rosacea can be a tricky, frustrating skin condition – but not every solution has to feel like a gamble. What makes blue light therapy for rosacea stand out is how quietly it works behind the scenes: lowering inflammation, calming visible redness, and slowly building your skin’s resilience.
Here’s what to keep in mind as you move forward:
- 🔹 In the first 1–2 weeks, you’re looking for signs of stabilization – less burning, less reactive skin, and a gentler flush response.
- 🔹 By weeks 3–6, consistent sessions (2–3x weekly) help space out flare-ups and reduce cytokine-driven inflammation.
- 🔹 For subtype 1 rosacea, blue light supports vascular calm without triggering rebound redness.
- 🔹 In subtype 2, it offers modest sebum balancing – helpful if pustules or oily areas accompany your flares.
- 🔹 The right blue light therapy time is short, measured, and low-dose. Don’t push too fast. Rosacea always does better with a slow-and-steady rhythm.
- 🔹 If you’re in an active flare or using photosensitizing meds, pause before starting.
Most importantly: you’re not trying to “fix” rosacea overnight—you’re teaching your skin how to react less and recover better.
Next Up: Blue Light for Oily or Seborrheic-Prone Skin
Think blue light is just for breakouts or redness? Not quite.
In our next post, we’ll explore how this gentle tech can help rebalance oily or seborrheic-prone skin – the kind that looks shiny by noon, flakes around the nose, or swings wildly with weather changes. You’ll learn how to time the oil shift, support your barrier, and avoid the dryness spiral that often follows over-cleansing.
If your skin feels both oily and irritated, this one’s for you.